
What Are Sensory-Based Feeding Issues?
Sensory-based feeding issues occur when a child has difficulty processing sensory information related to food. This can manifest in various ways, such as refusing to eat certain textures, becoming anxious during mealtimes, or exhibiting extreme reactions to specific smells or tastes. These challenges can stem from a variety of factors, and understanding the underlying causes is essential for effective intervention.
Signs of Sensory-Based Feeding Issues
Parents and caregivers should be on the lookout for signs of sensory-based feeding issues, which may include:
- Refusal to eat certain textures: Some children may reject foods that feel slimy, crunchy, or grainy.
- Aversion to smells: A child may refuse to eat foods simply because they dislike their smell.
- Limited food variety: Children with sensory-based feeding issues often have a restricted diet consisting of a few preferred foods.
- Gagging or choking: This may happen with textures the child finds intolerable.
- Heightened anxiety around food: Mealtimes may become a battleground, filled with stress and resistance.
If you notice these behaviors in your child, it may be time to seek professional help and Michigan Pediatric Therapy (MPT) in Farmington Hills, MI, is here to support you and your child.
The Link Between Sensory Processing Disorder (SPD) and Feeding Issues
Sensory Processing Disorder is a condition that affects how the brain processes sensory information. Children with SPD may be overly sensitive to certain stimuli or may seek out excessive sensory input. This can lead to challenges in various areas, including feeding.
How SPD Affects Feeding
Children with SPD might struggle with feeding for several reasons:
- Overreacting to Sensory Input: Children with sensory aversions may find certain textures, tastes, or smells overwhelming, leading to food refusal or anxiety during meals.
- Underreacting to Sensory Input: Conversely, some children may not react appropriately to hunger or fullness cues, leading to overeating or an irregular eating schedule.
- Negative Experiences with Food: A history of negative experiences related to food—such as being force-fed or experiencing gastrointestinal discomfort—can lead to long-lasting aversions.
- Underlying Conditions: Conditions like autism spectrum disorder, cardiac issues, or gastroesophageal problems (such as GERD or eosinophilic esophagitis, EoE) can exacerbate sensory feeding difficulties, making it harder for a child to engage with food positively.
Understanding these connections is crucial in addressing sensory-based feeding challenges.

Causes of Sensory-Based Feeding Issues
Negative Experiences with Food
Underlying Conditions
Certain medical conditions can also play a significant role in feeding issues:
- Autism Spectrum Disorder (ASD): Children with ASD often have sensory sensitivities that can manifest as feeding challenges, including extreme preferences for specific food types or textures.
- Gastroesophageal Issues: Conditions like GERD can make eating uncomfortable or painful, leading to aversions to food. Children may learn to associate mealtime with discomfort, creating a cycle of avoidance.
- Cardiac Issues: Children with heart problems may have feeding difficulties due to fatigue or energy conservation needs.ng a variety of foods.
Force Feeding
The Role of Pediatric Feeding Therapy
Pediatric feeding therapy is specifically designed to address feeding difficulties in children, particularly those related to sensory processing issues. An occupational therapist trained in feeding therapy, like ours at MPT, can work with families to create effective strategies to overcome these challenges.
How Pediatric Feeding Therapy Works
Assessment:
One of our licensed occupational therapists (OT) will conduct a comprehensive evaluation of the child’s feeding behaviors, sensory sensitivities, and overall development. This assessment helps identify specific feeding challenges.
Individualized Treatment Plan:
Based on the assessment, the OT creates a tailored intervention plan that targets the child’s unique needs. This may involve setting goals for expanding food variety, improving texture tolerance, or decreasing anxiety around mealtime.
Gradual Exposure:
Family Involvement:
Monitoring Progress:
The Importance of Occupational Therapy
Occupational therapy is instrumental in helping children develop skills for daily living, including feeding. Our OTs specialize in feeding therapy and focus on improving a child’s sensory processing abilities, motor skills, and overall relationship with food.
Benefits of Occupational Therapy in Feeding Issues
- Holistic Approach: Our OTs consider the child’s overall development, including sensory processing, motor skills, and emotional well-being, which can all impact feeding behavior.
- Skill Development: Our occupational therapists work on fine motor skills necessary for self-feeding, promoting independence in feeding tasks.
- Creating Positive Associations: Our OTs aim to help children develop a positive relationship with food by reducing anxiety and increasing comfort levels with different textures and tastes.

Practical Strategies for Parents and Caregivers
As a parent or caregiver, you can support your child’s feeding journey in several ways:
- Create a Positive Mealtime Environment: Ensure that mealtimes are calm and enjoyable, limiting distractions and encouraging family members to sit together during meals.
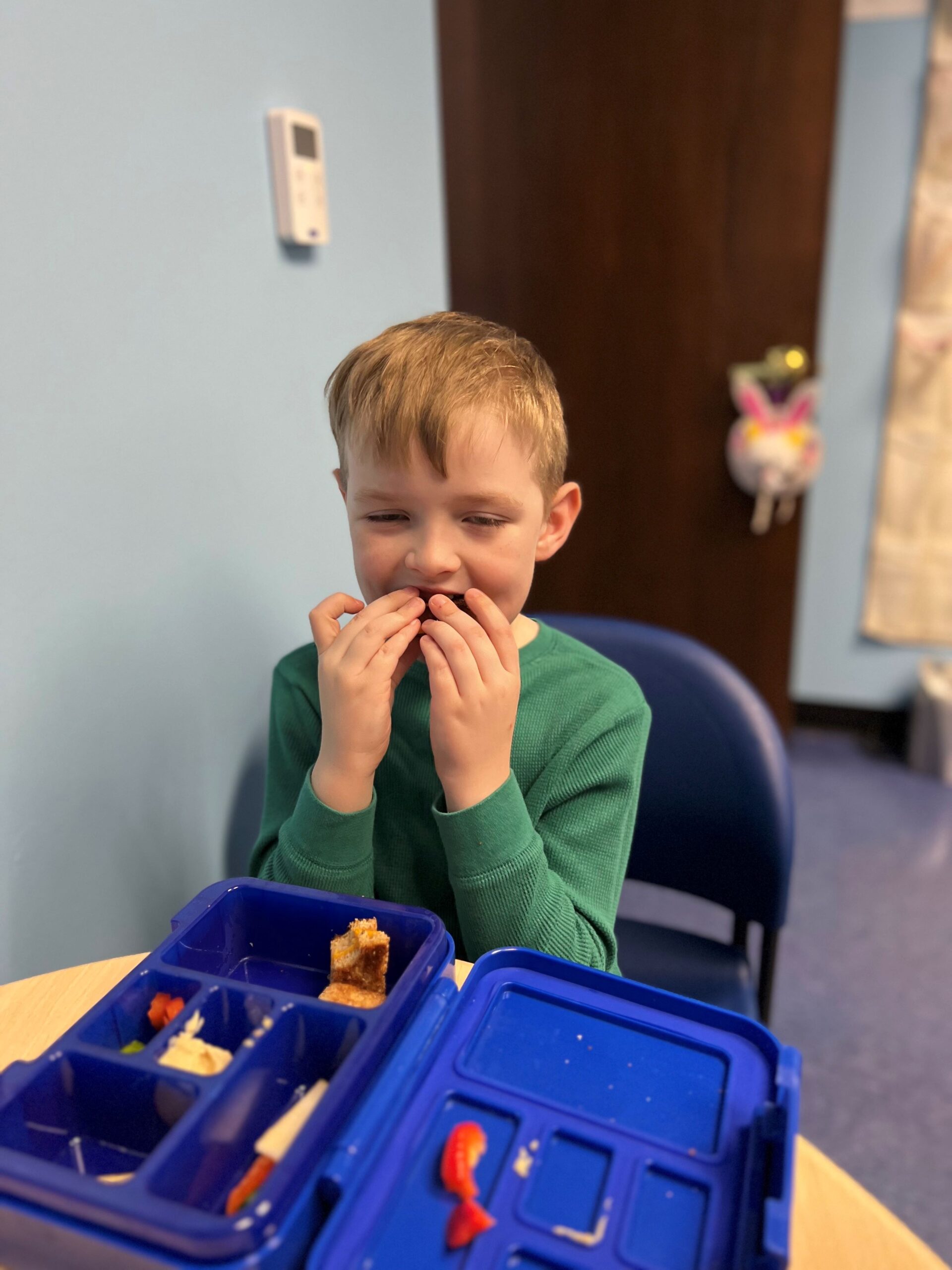
- Use Play to Explore Food: Allow your child to explore food through play. Encourage them to touch, smell, and manipulate different foods before trying to eat them.
- Be Patient: Changes in feeding habits take time. Celebrate small victories and avoid putting pressure on your child to eat.
- Offer Choices: Providing options can empower children and reduce mealtime battles. Allow them to choose between two healthy foods to encourage independence.
- Maintain a Routine: Consistent meal and snack times can help create a sense of security and expectation around food.
When to Seek Professional Help
If your child continues to struggle with feeding despite your efforts, it may be time to consult your child’s pediatrician to discuss if an evaluation with a feeding specialist is warranted. Early intervention is crucial in addressing sensory-based feeding issues and can lead to better outcomes for your child’s health and development.
Signs You Should Consider Consulting a Professional
- Persistent refusal to eat a variety of foods
- Significant weight loss or poor weight gain
- Excessive gagging or choking during meals
- Heightened anxiety around food and mealtime
- Limited food variety beyond typical picky eating behaviors

Conclusion
Sensory-based feeding issues can significantly impact a child’s well-being and development. Understanding the link between sensory processing disorder and feeding difficulties is crucial for parents and caregivers. By seeking help from pediatric feeding therapy and occupational therapy, families can implement effective strategies to address these challenges, making mealtimes less stressful and more enjoyable.
If you have concerns about your child’s feeding habits or sensory processing, consider reaching out to our team at Michigan Pediatric Therapy. Our experienced occupational therapists are here to provide personalized guidance and support for your family.
Michigan Pediatric Therapy
📍 27655 Middlebelt Rd., Suite 130, Farmington Hills, MI 48334
📞 (248) 939-4030
🌐 mipediatrictherapy.com
References
- American Speech-Language-Hearing Association. (n.d.). Feeding and Swallowing Disorders. Retrieved from ASHA.
- McGowan, J., & Nuttall, C. (2018). Feeding Difficulties and Their Management. Journal of Pediatric Health Care. Retrieved from JPHC.
- American Academy of Pediatrics. (2016). Gastroesophageal Reflux: Management of Gastroesophageal Reflux in Infants and Children. Retrieved from AAP.
- American Occupational Therapy Association. (n.d.). Pediatric Feeding and Swallowing. Retrieved from AOTA.
- Cohn, E. S., & Tonniges, T. (2018). Improving Feeding Skills in Children with Sensory Processing Disorder. The American Journal of Occupational Therapy. Retrieved from AJOT.



